Introduction
Itchy, flaky scalp conditions are common, but not all scalp flaking is the same. Many individuals confuse dandruff, seborrheic dermatitis, and scalp psoriasis, yet each has distinct causes, patterns, and implications for long-term scalp and hair health. Misidentifying these conditions can delay proper management and worsen symptoms.
This article outlines the differences between these three scalp disorders, how they affect hair and scalp health, and why a trichological perspective is essential for accurate evaluation.
Dandruff: The Mildest Form of Scalp Flaking
Dandruff is considered the mildest expression of scalp flaking. It is primarily caused by an overgrowth of Malassezia yeast, which irritates the scalp and accelerates shedding of dead skin cells (Borda & Wikramanayake, 2015).
Key features of dandruff include:
- White or gray flakes that are loose and easily brushed from the scalp.
- Mild itching without significant redness or inflammation.
- Typically confined to the scalp, without spreading to other areas of the body.
Dandruff is largely cosmetic but can progress to seborrheic dermatitis if scalp inflammation increases.
Seborrheic Dermatitis: A Chronic Inflammatory Condition
Seborrheic dermatitis (SD) is a more advanced inflammatory form of dandruff. Like dandruff, it is associated with Malassezia overgrowth, but additional factors — such as immune response, barrier dysfunction, and excess sebum — contribute to its persistence (Clark et al., 2015).
Key features of seborrheic dermatitis include:
- Yellowish or greasy scales that adhere to the scalp.
- Red, inflamed patches underneath the scaling.
- Itching that is more intense than dandruff.
- May affect other sebaceous-rich areas such as eyebrows, ears, and chest.
Unlike dandruff, seborrheic dermatitis is a chronic condition that often recurs without continuous management.
Scalp Psoriasis: An Autoimmune Disorder
Scalp psoriasis is fundamentally different from both dandruff and seborrheic dermatitis. It is an autoimmune disease in which the immune system accelerates the skin cell turnover cycle, leading to thick, adherent plaques (Nestle et al., 2009).
Key features of scalp psoriasis include:
- Thick, silvery-white scales that may extend beyond the hairline.
- Well-demarcated patches with significant redness and inflammation.
- Possible bleeding when scales are removed (“Auspitz sign”).
- May coexist with psoriasis elsewhere on the body (elbows, knees, nails).
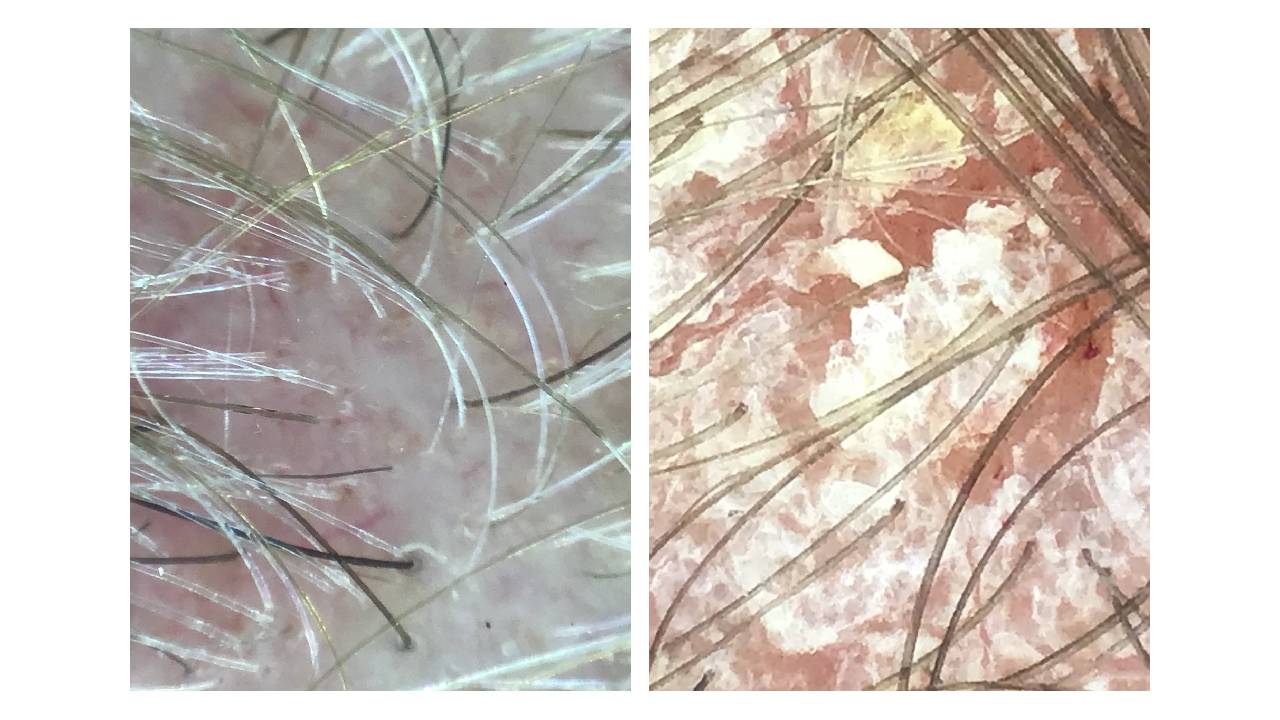
Scalp psoriasis can be mistaken for seborrheic dermatitis, but the plaques are typically thicker, more defined, and extend beyond the scalp. Importantly, psoriasis is systemic, with immune and inflammatory implications beyond the scalp.
Impact on Hair and Scalp Health
While dandruff alone does not cause permanent hair loss, both seborrheic dermatitis and scalp psoriasis can create environments that weaken follicles over time:
- Chronic inflammation damages the follicular environment, making hair more prone to shedding.
- Barrier disruption increases susceptibility to infection or secondary inflammation.
- Psychological impact can increase stress, which itself may worsen shedding.
From a trichological perspective, managing these disorders involves more than symptom relief. Supporting scalp balance, reducing inflammation, and addressing systemic contributors (such as immune or gut dysfunction) are essential for preserving long-term follicular health.
How to Tell Them Apart
While these conditions overlap, several distinguishing features can guide identification:
- Dandruff: Loose, white flakes with mild itching, no redness.
- Seborrheic Dermatitis: Greasy yellow scales with underlying redness and more intense itching.
- Psoriasis: Thick silvery plaques, sharp borders, often spreading beyond scalp.
However, proper diagnosis may require professional evaluation, as mixed presentations are common. Trichoscopy and scalp analysis can provide additional insights into scaling patterns and follicular involvement.
Conclusion
Dandruff, seborrheic dermatitis, and scalp psoriasis are distinct conditions that share overlapping features but differ in cause, severity, and long-term implications. Understanding these differences is critical for appropriate management and prevention of hair loss.
For those struggling with persistent scalp flaking, professional evaluation through a trichologist or dermatologist is recommended to determine the underlying condition and create a tailored management plan. Functional trichology adds another layer by examining not only the scalp but also systemic factors — such as immune function, diet, and stress — that influence scalp health.
References
Borda, L. J., & Wikramanayake, T. C. (2015). Seborrheic dermatitis and dandruff: A comprehensive review. Journal of Clinical and Investigative Dermatology, 3(2), 10.13188/2373-1044.1000019.
Clark, G. W., Pope, S. M., & Jaboori, K. A. (2015). Diagnosis and treatment of seborrheic dermatitis. American Family Physician, 91(3), 185–190.
Nestle, F. O., Kaplan, D. H., & Barker, J. (2009). Psoriasis. New England Journal of Medicine, 361(5), 496–509. https://doi.org/10.1056/NEJMra080459

